Claims view lists all the claims and pre-authorization requests created for procedures related to each patient.
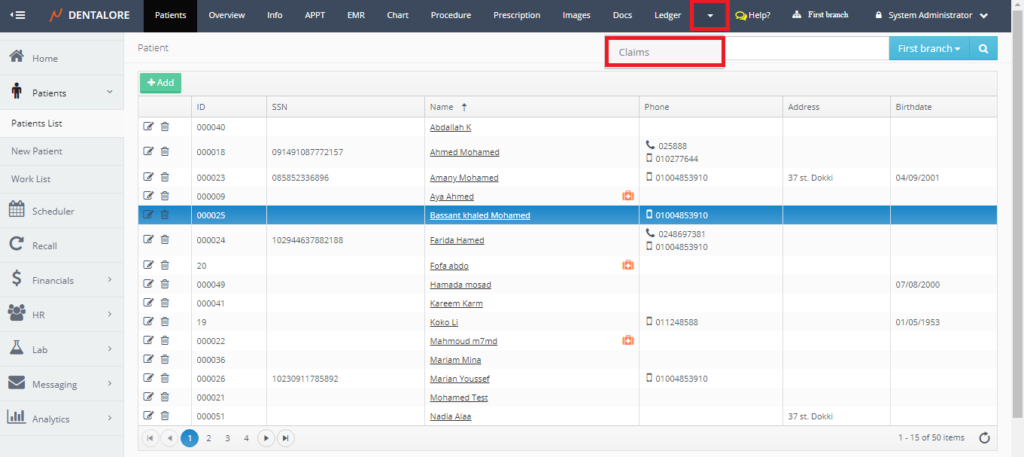
To Access the Claims View, Follow the following:
- Expand "Patients" menu and Select "Patient List".
- Select any of the existing patients (Who has Insurance to find claims) and then Select "Claims".
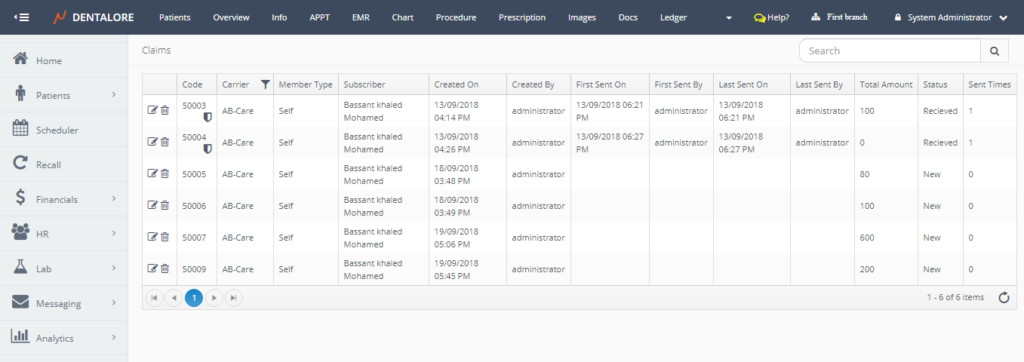
Claims View contains: Search Area and a grid view displays all claims and pre-authorization created for the selected patient.
1- Search Area
User could search for a specific claim using the: Claim Code, Patient ID, Patient Name, or Carrier.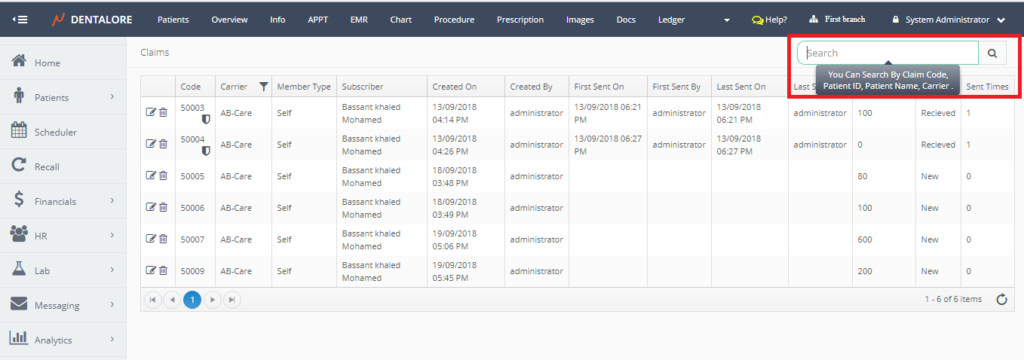
2- Claims Grid View
- Actions Column: 2 actions could be performed on the Claim and Pre-authorization Transactions:
-- "View" Icon: Once Pressed, User is directed to "Claim Details" page in order to manage all information related to the selected claim or pre-authorization. For more information, Check: Claim Transaction.
-- "Delete" Icon: Once Pressed, Popup "Delete Claim" Opens.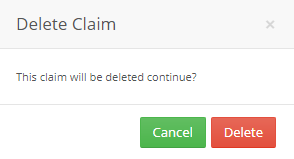
-- If user Press "Cancel" button then the Claim will not be deleted and still displayed in the Claims grid view. If user Press "Delete" button then the selected Claim will be deleted. - Carrier: Is the name of the insurance company that deals with the patient.
- Member Type: Is the relation to the selected patient with his/her family.
- Subscriber: Is the name of the person who is the subscriber for the insurance.
>> Note that: When the "Member Type" is (Self) then the "Subscriber" displays the patient's name. - Created On: Is the date when the claim has been created.
- Created By: Is the name of user who created the claim.
- First Sent On: Is the date when the claim sent to the insurance company for the first time. Sending claim is performed from the "Claim Details" page.
- First Sent By: Is the name of the user who sent the claim to the insurance company for the first time.
- Last Sent On: Is the date when the claim re-sent to the insurance company. Re-sending claim is performed from the "Claim Details" page.
- Last Sent By: Is the name of the user who re-sent the claim to the insurance company.
- Total Amount: Is the total amount of money included in the claim that insurance should pay.
- Status: Is the Status of the claim or pre-authorization transaction. Status differs if the transaction is a pre-authorization or a claim as follow:
-- For the Claim, Status could be: (New, Sent, Accepted, Rejected, Received, or Closed) and user is able to update it from the "Claim Details" page.
-- For the Pre-Authorization, Status Could be: (New, Sent or Received) and user is NOT able to update it from the "Claim Details" page.
>> Note that the transaction of status "Sent" can't be deleted. - Sent Times: Is the count of how many times did the selected claim has been sent to the insurance company.
