For the patients who have insurance, the user could create a pre-authorization for the required procedures to be sent to the insurance company before sending a claim.
Pre-Authorization is managed from the “Chart” view; “Treatment Plans” tab.
To Create a Pre-Authorization, Follow the following:
- Expand the “Patients” menu and select “Patient List”.
- From the patients grid view select any of the existing patients (Who have insurance).
- All patients’ modules become enabled, Select the “Chart”.
- Select “Treatment Plans” tab.
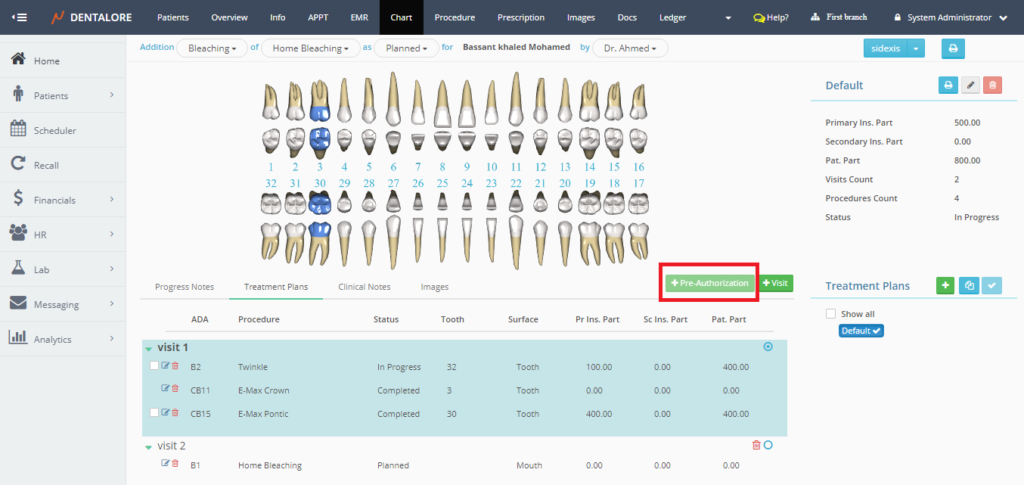
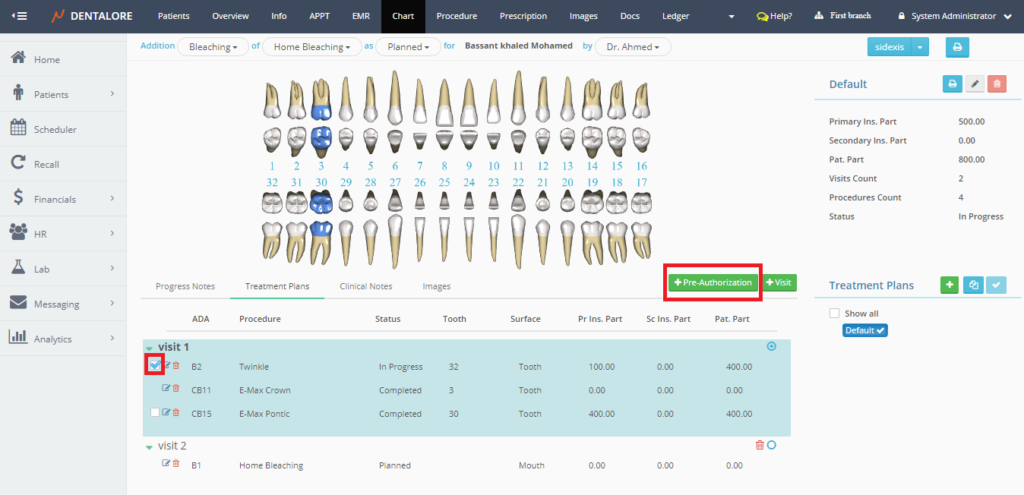
- By default the “Pre-Authorization” button is disabled. User must tick on the check box of required procedures to activate the “Pre-Authorization” button.
- Press the “Pre-Authorization”.
- New “Create New Pre-Authorization” popup appears, that lists the procedures requested for the pre-authorization with it’s data (ADA Code, Name, Status, Tooth Number, Surface, Primary insurance part, Secondary insurance part and the patient part).
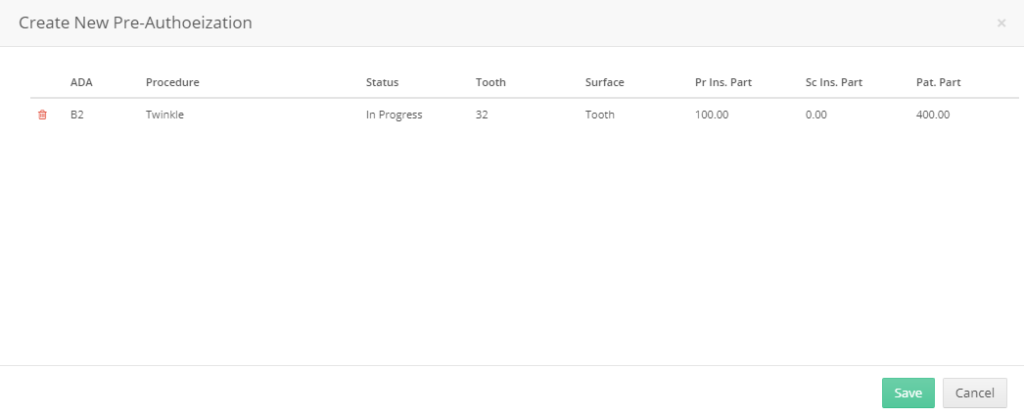
- If user press “Cancel” button, then the “Pre-Authorization” will not be created and popup closes.
- If user press “Save” button, then the following occurs:
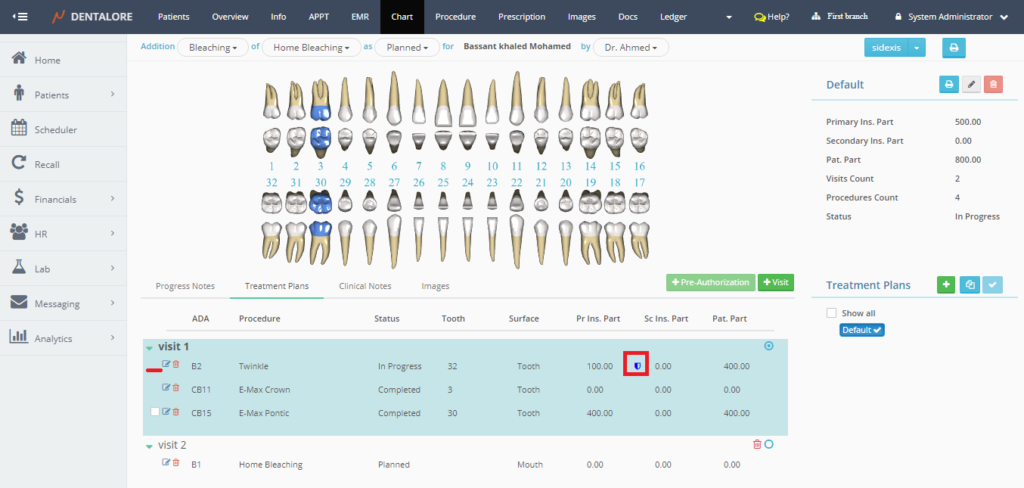
— “Pre-Authorization” will be created and listed in the “Claims” View to perform the required actions towards the insurance company,
— Popup closes
— The check box beside the selected procedure removed.
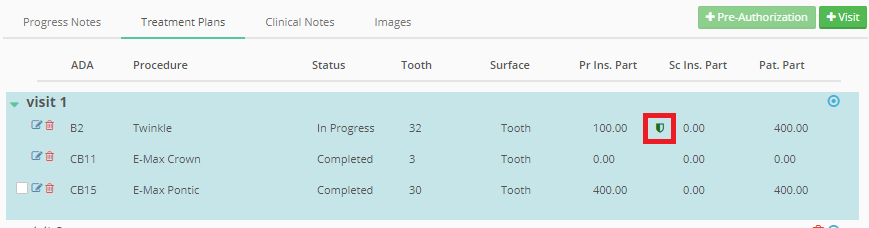
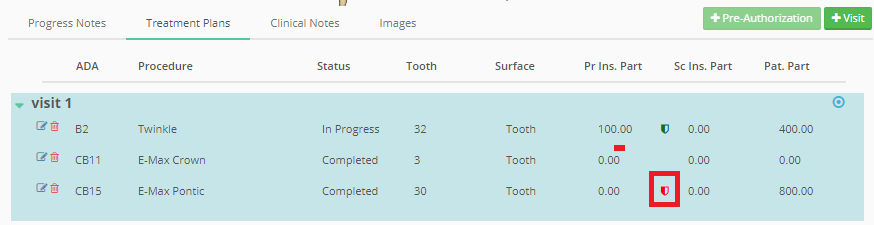
— New Symbol appears beside the Primary insurance part in Blue color which means that a pre-authorization had been created for this procedure.
- From the “Claims” view, user could sent the pre-authorization then insurance company accept or reject the request.
— if the pre-authorization request is accepted, then the color of “Pre-Authorization” Symbol in “Treatment Plans” tab changed from Blue to Green.
— if the pre-authorization request is rejected, then the color of “Pre-Authorization” Symbol in “Treatment Plans” tab changed from Blue to Red.
- Note that once a pre-authorization is accepted or rejected, it can’t be edited or change it.
>> For more information about managing the “Pre-Authorization” from Claims view, Check: Pre-Authorization Management from Claims View.
